SEPTEMBER 30, 2020
. . .
Treating a patient’s immediate clinical needs isn’t enough to fully care for them.
There are non-medical factors in a person’s life that affect their health and overall well-being — and whether you’ll be seeing them again sooner than planned.
Called social determinants of health1 (SDOH), these factors can include:
- A community’s social landscape
- The quality and safety of physical environments
- Risky activities and behaviors
- The accessibility of medical care
- A person’s education and economic status
Even though these factors are beyond your control after a patient is discharged, there are simple ways your teams and your patient technology can help address SDOH.
Let’s explore each area of social determinants, and how your hospital can prepare patients for a successful transition of care.
Social determinant of health:
Education level
Whether a person has early childhood education, graduated high school or attended higher education impacts their ability to understand the significance and address the needs of their health or condition.
Patients may also have poor literacy skills, language barriers or a lack of engagement in their care plans that affect their health outcomes.

What can your team do to help?
Communicate, educate and teach back.
In-room displays can communicate information in different languages to assist patients with language barriers.
Bedside interpreter services can help ensure clear communication between patients and providers when it comes to understanding what to do for themselves or a family member.
A PAM (Patient Activation Measure) assessment can be placed on the system to help providers determine the level of a patient’s engagement in their health and well-being.
SONIFI Health’s nursing executives can consult with your teams on the needs of your patient population, and recommend specific education content to address their conditions, preventive or safety measures, medications and more.
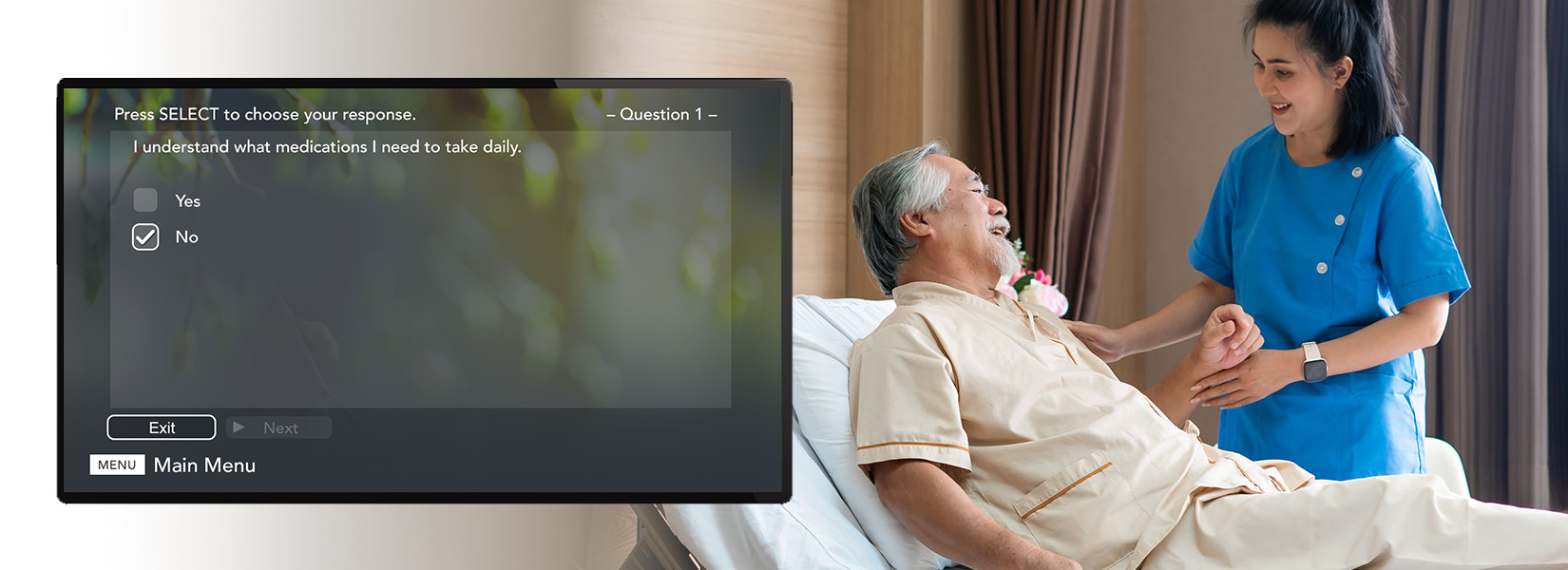
On-screen prompts can encourage a patient to complete their education assignments, and the results of comprehension surveys can flag if the care team needs to discuss more with the patient.
Social determinant of health:
Neighborhood & built environments
A neighborhood’s environmental conditions like polluted air, contaminated water and extreme weather can contribute to increased risks of cancers, illnesses, injuries and chronic conditions.
The quality and maintenance of a person’s home — the air quality, presence of mold or asbestos, space per individual, structural safety, etc. — can also impact their physical and mental health.
A community’s prevalence of crime and violence, and its availability of nutritious foods (e.g., food deserts), can influence a person’s mental health and physical well-being as well.
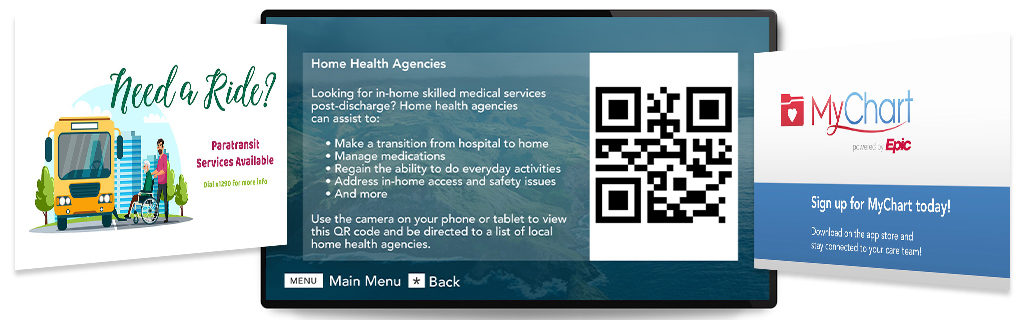
Link community resources for food, safety and housing via the in-room TV or QR code.
What can your team do to help?
Provide education and resources.
SONIFI Health’s platform can link to community resources for nutrition, safety and housing via the Information feature or QR codes. A custom TV channel on the system can be used as a dedicated “discharge channel” that loops community resources available post-discharge.
We can also recommend education videos about wellness and nutrition that may be beneficial to assign to patients, and place surveys on the system that ask patients what concerns they have, with responses automatically routing to a specific department, such as social work, to follow up.
Social determinant of health:
Community & social context
A person’s experiences with discrimination regarding their race, gender, religion, age, disability, sexual orientation, incarceration history, etc., as well as their level of social cohesion (e.g., emotional support, healthy relationships, solidarity with community members) and civic participation (e.g., voting, volunteering, community involvement) can significantly impact their health.
Without positive social support and interactions, a person can become isolated and depressed. In addition to detrimental effects on their emotional and psychological well-being, socially isolated people tend to not report health issues or participate in health prevention and screenings, and they’re less likely to seek medical care or treatment for chronic health issues.
What can your team do to help?
Connect patients with resources.
The Request and Information features on SONIFI Health’s platform can be used to highlight and promote community resources and programs that patients can use for help with discrimination issues, preventive health, therapy, drug treatment and many other areas depending on what assistance is available in your area.
Our nursing executives can also recommend education content about wellness, screenings, mental health and more to address your patient population needs. Our platform is designed to engage and empower patients to view the education titles assigned by your care team.
Internally, also ensure your organization’s trainings and protocols regarding discrimination, implicit bias, diversity, health equity and inclusion are promoted and up to date with your clinicians.
Social determinant of health:
Economic stability
A person’s economic stability is affected by:
- Their employment status, including salary and hours available to work
- If they have debts like credit card bills, medical bills and student loans
- If their income can cover essential needs like housing, food, utilities, transportation, medications and healthcare
- Their access to assistance if they have financial issues
If a person’s basic needs cannot be met financially, it can lead to food insecurity, housing instability, poverty and homelessness.
What can your team do to help?
Ask patients about these economic factors, and connect them with resources for assistance.
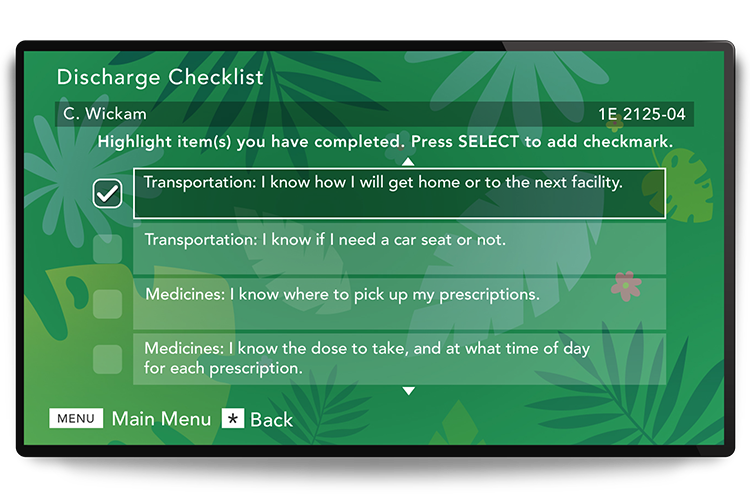
Clinicians can use SONIFI Health’s platform to identify a patient’s needs through customizing the Discharge Checklist, Survey, or Request features.
Automations can flag your social workers to follow up with the patient, and use in-room technology to display the website and contact information for relevant community resources, such as food banks, housing classes, job skills programs, career counseling or local child care programs.
Social determinant of health:
Healthcare accessibility
Unreliable transportation, inadequate health insurance, no insurance, high out-of-pocket costs, existing medical debt and limited access to care — such as long wait times, long distances, incompatible scheduling and lack of providers — can all lead a person to not seek care until it becomes a crisis, and to be less likely to receive and follow through with preventive care for chronic conditions.
A person’s health literacy2 can also affect their outcomes. Literacy, being able to read and write, is different than health literacy, which refers to a person’s capacity to obtain and understand the information needed for them to take appropriate actions for their health.
Patients with low health literacy are less likely to adhere to a medication regimen, and more likely to use the emergency department when seeking care — and to return to the emergency department within two weeks of the first visit.
What can your team do to help?
Communicate and teach back at the patient’s health literacy level.
SONIFI Health’s platform can help caregivers assess a patient’s literacy level with a survey/feedback tool, and integrate relevant EHR data. Our team can also recommend patient education videos that are done at a level patients can easily understand.
The effects of addressing a patient’s social determinants of health
Think of SDOH as a wheel: Each part must be in place and in good shape for the wheel to function properly.
A person must have all domains of social determinants in place3 to have good health and positive health outcomes. And when your patients are successful, they’re less likely to be readmitted — and reimbursements, the overall cost of healthcare and the quality of your community improves for everyone.
Programs like the CMS Accountable Health Communities Model4 and Medicare Advantage preventive expansions5 are leading the way in showing the value of healthcare organizations addressing SDOH.
This takes intentional effort, but it doesn’t have to require huge institutional change.
Simply incorporating screening tools6 into clinical workflows and asking patients about their situation can make a big difference in how your care can extend beyond your facility.
Capturing a patient’s social determinants early in their hospital stay allows for more effective discharge planning and potentially impacts their length of stay. EHR integrations with SDOH data can more accurately calculate a patient’s risk of readmission score.
Use the ICD-10 Z codes7 in your EHR to indicate what assistance is needed, and leverage the SONIFI Health system to establish automations that:
- Send messages to your discharge planner, social worker or other team to make additional arrangements
- Deliver relevant and effective education to patients
- Survey patients for feedback, comprehension and specific needs
- Alert the care team if teach backs or additional conversations are needed
- Display community resources that are available
- Provide easily accessible medication instructions, program contact information and more for patients to reference
The better you can help set up patients for success post-discharge — by addressing their social needs as well as their clinical needs — the more likely they are to achieve their best health and quality of life.
Stay connected
Get exclusive insights delivered to your inbox from our experts.
 By SONIFI Health
By SONIFI Health